Global Standards for Midwife Faculty Development – Companion Guidelines

The ICM Global Standards for Midwife Faculty Development are an essential component of ICM’s efforts to strengthen midwifery education worldwide. These standards are a core ICM document and one of the ICM Midwifery Education Development Pathway (MPath) resources, which include standards, guidelines, definitions, position statements and tools related to midwifery education. High standard midwifery education is essential to producing competent midwives for the future midwifery workforce, providing safe and culturally appropriate care to women, newborns and their families. Appropriately prepared midwife faculty are the backbone of quality midwifery education programmes.
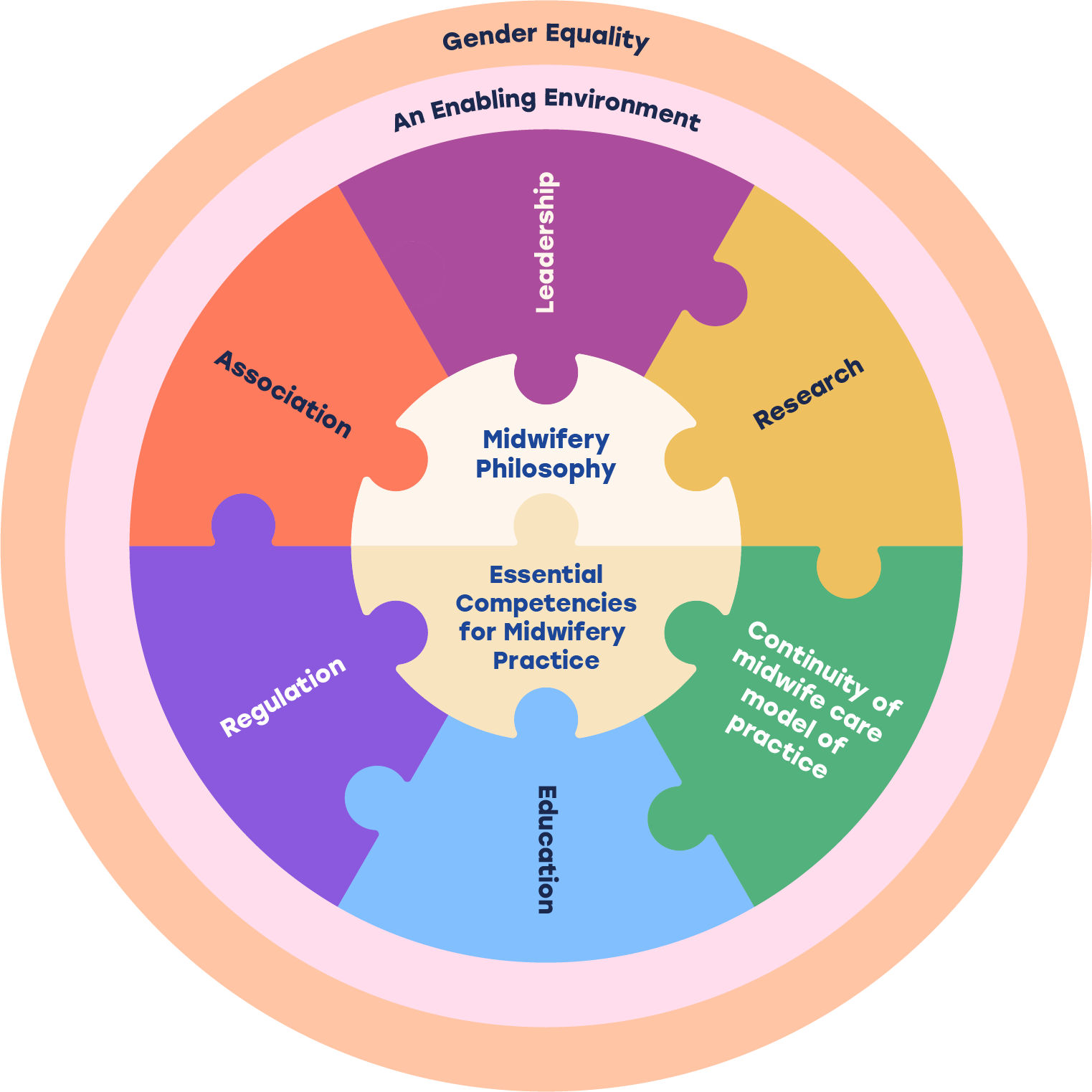
The ICM Global Standards for Midwife Faculty Development reflect foundational ICM Core Documents including the Definition and Scope of Practice of a Midwife, the Midwifery Philosophy and Model of Practice. They align with the ICM Global Standards for Midwifery Education and the WHO Midwifery Educator Core Competencies. The standards set out the knowledge, skills and experience that midwife educators and clinical preceptors should receive through quality midwife faculty development as preparation for their teaching roles.
Midwife faculty are registered and professional midwives. As such, they should already meet the ICM Essential Competencies for Midwifery Practice, work to the ICM Midwifery Philosophy and meet ethical standards set by the relevant in-country regulator as part of the midwife registration process. The ICM Global Standards for Midwife Faculty Development build on the competencies, philosophy and ethics of the midwifery profession with focus on the areas of development required for those midwives working as faculty or clinical preceptors and teaching the next generation of midwives.
The purposes of the ICM Global Standards for Midwife Faculty Development are to:
- set benchmarks and quality indicators for midwife faculty development,
- provide a framework for designing, implementing and evaluating midwife faculty development,
- assist midwife faculty to engage in continuous quality improvement process,
- contribute to strengthening midwifery education programmes globally through preparing and improving the capacity of midwife faculty.
Additionally, the ICM Global Standards for Midwife Faculty Development (2025) may be used by educational institutions/providers to:
- support faculty development;
- support in-service continuing education (e.g., opportunities) and/or inform a faculty development programme within an institution; and
- meet national and global approval and accreditation standards.
The Global Standards for Midwife Faculty Development provide the minimum standards for quality midwife faculty development. ICM recognises that educational institutions may be at different levels of maturity regarding faculty development and may be supported by other stakeholders (e.g., Regulators, Ministry of Health/Education, Midwives’ Associations, NGOs) in the development and implementation of midwife faculty development programmes and activities. Regardless of stakeholder requirements, ICM recommends that all midwife faculty development be based on the requirements of midwife faculty, as the primary recipients of development programmes. Consideration should also be given to the needs of midwife students as the direct recipients of teaching from midwife faculty and the needs of women and gender diverse people receiving sexual, reproductive, maternal, newborn and adolescent healthcare services (SRMNAH) from midwives. To meet such diverse needs, the ICM recommends conducting a needs assessment/analysis particularly of midwife faculty, midwife students and the SRMNAH context. The findings of this needs analysis can be used to determine the most effective faculty development activities to support midwife faculty attain competence as teachers and to prepare competent midwife graduates to provide quality care for women and newborns.
This document serves as a companion to the ICM Global Standards for Midwife Faculty Development, providing supplementary information and insights.