Midwifery Models of Care – built on community engagement and interprofessional collaboration

This is the second in a series of articles on Midwifery Models of Care. In the first article we explored the substantial and long-awaited boost in recognition for the midwifery profession and women’s right to respectful care as a result of the release of the WHO Global Position Statement on Transitioning to Midwifery Models of Care and The Midwifery Accelerator. In this article we will further explore the importance of the Implementation Guidance on Transitioning to Midwifery Models of care launched by ICM, UNICEF, UNFPA, WHO and collaborating partners on 18 June 2025.
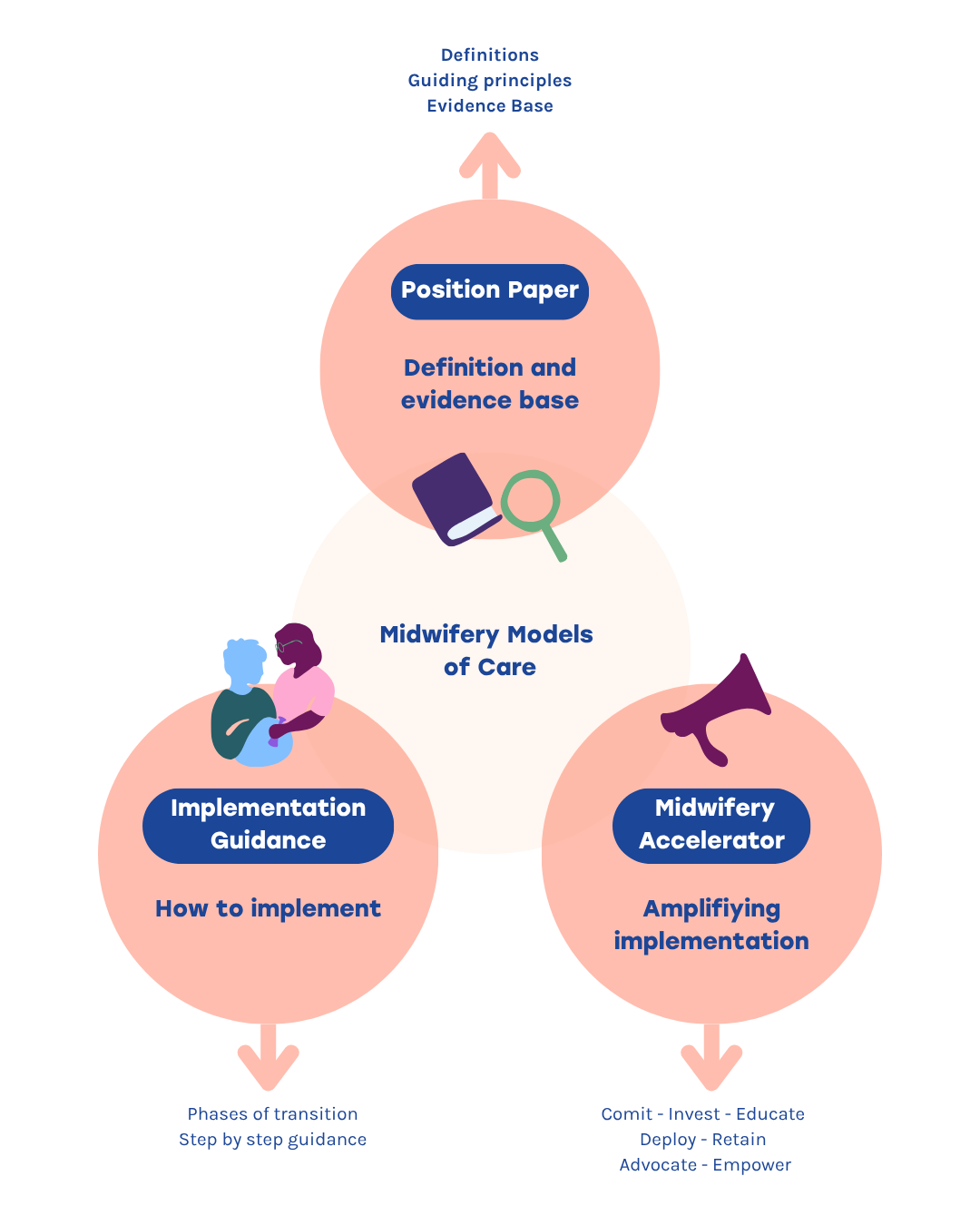
The graphic below shows how the three documents are connected.
Implementing Midwifery Models of Care
Midwifery Models of Care have been identified as a global health best-buy for many reasons, including:
- improved health outcomes,
- increased access to maternal and newborn health services and sexual and reproductive health and rights,
- improved experience and satisfaction for women,
- to maximise resource efficiency and as a contributing factor to social and economic development and gender equality.
The Implementation Guide offers strategic and practical advice, along with actionable steps for integrating and enhancing midwifery care within national and sub-national health systems. The Guidance is designed for policy-makers and health care leaders, identifying a broad range of stakeholders needed for success, including service-users, midwives, associated health professionals, professional associations, and regulatory authorities
Midwives – a smart investment
Midwives are an essential component of cost-effective, high-quality investments in efforts to improve maternal and newborn health outcomes.
Midwifery Models of Care are models in which the main care providers for women and newborns, starting from pre-pregnancy and continuing all the way through the postnatal period, are educated, licensed, regulated midwives autonomously provide and coordinate respectful, high-quality care across their full scope of practice, using an approach that is aligned with the Midwifery Philosophy of Care.
Midwifery models of care offer the flexibility to adapt to various delivery platforms, including community, hospital, public, private, and humanitarian or crisis settings. The model of care is not standardised, but can be altered to meet the specific needs of a country or context. This customised approach with the midwife as the main care provider has resulted in a diverse range of midwifery models of care worldwide.
Examples of adaptable configurations of Midwifery Models of Care are:
- Continuity of midwife care models: a known and trusted, or a small team of midwives acting as the primary caregiver throughout the entire continuum of care.
- Community-based models: care delivered directly to local communities.
- Birth centres: dedicated spaces where midwives provide intrapartum care and other services for women at low risk of complications.
- Private practice models: increasing community access to midwives integrated into and financed by national or sub-national health systems.
- Models for humanitarian and crisis settings: flexible, mobile solutions to meet maternal and newborn health care needs in resource-constrained environments.
Strategic planning
The Guidance emphasises engaging in partnerships, securing political commitment and funding, strengthening governance, and employing a high-level strategy to ensure sustainable transition to Midwifery Models of Care. These essential pillars for transition are supported by a strategic four-step planning process which includes: evaluating the current situation, establishing priorities, developing an operational plan, allocating resources, and ensuring a framework for continuous monitoring and evaluation.
Key transition areas necessary for a comprehensive approach to change are identified, with recommended actions being defined. These areas include community engagement, service delivery, interprofessional collaboration, leadership, research, education and continuous professional development, regulation, workforce optimisation, and infrastructure. The implementation process requires adaptability, and the guide includes a Transition Framework Assessment Tool designed to help countries review their current situation and take steps to transition to the next phase across these key areas. Additionally, case studies from five countries illustrate flexible approaches and context-specific solutions.
As with all documents containing strategic and practical guidance for health system change, stakeholders need to familiarise themselves with the approach and the content and take steps to contextualise the information to the local setting. This does involve the need for immersive reading and analysis of material and supporting documents.
But what type of shift in thinking is required for a midwife to become the main care provider across the continuum of maternal and newborn health services?
The following two sections describe the necessary changes in two key areas identified by the guide as critical for the success of midwifery care models: engaging women and communities, and interprofessional collaboration.
Engaging women and communities
Midwives are an invaluable resource for maternal and newborn care, yet their significance often remains underappreciated. A critical step in advancing midwifery models of care is ensuring that women are aware of the pivotal role midwives play but also recognise how their expertise directly benefits maternal and newborn health outcomes and exoeruences. Midwives offer more than medical proficiency; they provide a partnership centered on mutual respect and trust, empowering women by validating their autonomy and knowledge about their own bodies.
Community engagement plays an essential role in spreading awareness about these benefits. Women should be equipped with comprehensive information about how midwives can coordinate care services, promote healthy physiological processes, and serve as the main care provider throughout pregnancy, childbirth, and postnatal care. This awareness facilitates informed decision-making, ensuring women have access to choices that align with their needs and preferences.
Interprofessional collaboration
Effective maternal and newborn care relies on interprofessional collaboration. By fostering equal partnerships between midwives, obstetricians, paediatricians, and other allied health professionals, care systems can leverage the unique strengths of each discipline to deliver comprehensive and high-quality services. This collaboration is not about diminishing one profession to elevate another; rather, it is about enabling all professionals to work to the full scope of their practice.
When midwives are supported to exercise their expertise in promoting normal physiological processes and coordinating maternal and newborn care, they contribute to reducing unnecessary medical interventions. Concurrently, obstetricians and paediatricians are enabled to focus on complex-care needs, stepping in when specialised skills are required. Such a balanced approach ensures that every individual receives the most appropriate level of care tailored to their specific needs.
Crucially, this model relies on mutual respect and trust among professionals. Shared decision-making, transparent communication, and commitment to common goals to create an environment where each profession can thrive. The integration of midwives into interdisciplinary teams allows for dynamic care pathways, where seamless referrals and consultations ensure optimal outcomes for mothers and newborns. This model not only enhances the quality of care but also strengthens the foundation of healthcare systems by making them less resource intensive, more adaptable, and holistic.
A supportive health system environment
The implementation guidance aims to support the integration of key transition areas such as community engagement and interprofessional collaboration into health systems to achieve a transition to Midwifery Models of Care for optimal outcomes in maternal and newborn care. This requires support for midwives to coordinate care, make autonomous decisions, and work to their full scope of practice within collaborative teams.
The guide is designed to be adaptable for countries with varying needs, whether they are adopting midwifery models of care or scaling up existing services. Its primary focus is on creating context-specific health system environments equipped with functional and responsive infrastructures that support midwifery models of care. Practical steps are illustrated with success stories from transition countries.
The guide emphasises fostering partnerships among Ministries of Health, policymakers, healthcare administrators, professional associations, midwifery educators, practicing midwives, and allied health professionals. This balanced approach ensures that all professions involved in maternity and newborn care can collaborate effectively, meeting the needs of women and communities while promoting best practices.
In the next, and final article in this series, we will explore different forms of Midwifery Models of Care and highlight the need for all countries to respond to the call to action by implementing innovative models that answer the challenges relevant to their context, strengthen the midwifery profession and expand choice for women and gender diverse people.
Given today’s highly political and deeply concerning global context, the world needs midwives more than ever. Health systems everywhere are under immense pressure, and we now know that investing in autonomous midwives and the midwifery profession is one of the best investments a country—or a donor—can make.